Prof. N. Reha Tandoğan, M.D. - Asım Kayaalp, M.D.Artificial joint replacement (arthroplasty, joint prosthesis) is a very successful operation for advanced damage to the joints. Although joint replacement provides excellent pain relief and acceptable function, it does not permit an active lifestyle, heavy labor or impact sports. Performing these high impact activities may cause early wear and loosening of the joint replacement and is discouraged. Joint preserving surgery is for middle aged patients with moderate damage to the joint who would like to continue their active lifestyle and do not want to accept the limitations of joint replacement.
Is joint preserving surgery suitable for me?
Joint preserving surgery is indicated for active young-middle aged patients with moderate arthritis who want to maintain their active lifestyle. This type of surgery aims to delay and sometimes avert total joint replacement for a reasonable period of time. Joint preserving surgery is not possible in advanced arthritis regardless of age, in which extensive involvement of all parts of the joint is observed. Joint preserving surgery has a limited role in rheumatoid arthritis and other inflammatory joint diseases. The recovery period is longer than a total joint replacement and requires a certain amount of regenerative potential, therefore is not suitable for elderly patients with chronic medical problems. Your orthopedic surgeon will decide if this type of surgery is suitable for you after a detailed physical examination, X-rays, magnetic resonance imaging and blood tests.What is joint preserving surgery?
Joint preserving surgery encompasses a variety of procedures that aim to restore or reconstruct the damaged parts of the joint. If the alignment of your leg is abnormal, a procedure called an “osteotomy” may be performed to unload the damaged compartment. One or two bones in the leg are cut, re-aligned and fixed with screws and plates during an osteotomy (Picture 1). This usually is a first step of joint preservation if your leg alignment is unfavorable and is mostly performed around the knee joint. An “osteoplasty” can be performed in the hip joint in patients with impingement syndrome. This is a procedure in which the impinging bone prominence is removed to prevent cartilage and labrum damage and is usually performed arthroscopically.
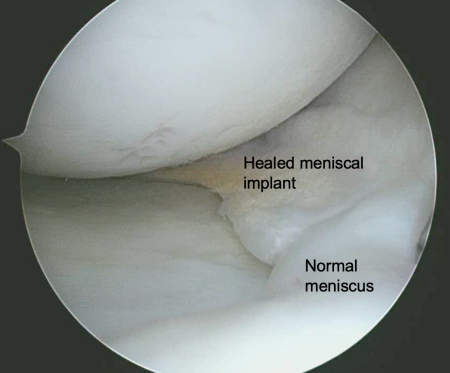
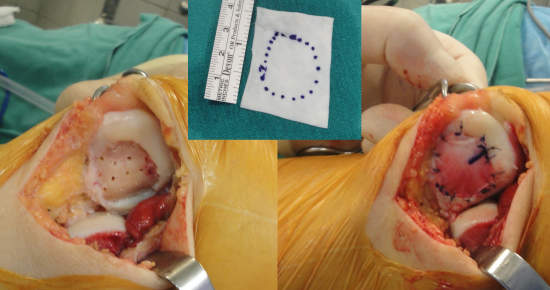
Another aspect of joint preserving surgery is meniscus repair or replacement in the knee joint. A specific type of tear called a root tear is frequently seen in patients with early degenerative arthritis. The meniscus is torn from its boney attachment and is extruded out of the joint, losing its capability to bear load and protect the cartilage (See “Treatment Options in Meniscal Root Tears Have Changed Radically in Recent Years” section in this web site). Repairing this tear restores the normal mechanics of the knee joint. If the meniscus is damaged beyond salvage, the meniscus can be reconstructed with “meniscal implants”. Meniscal implants are synthetic porous materials that are used to restore partially damaged menisci (Picture 2). If the meniscal damage is extensive, “meniscal allografts” (meniscal tissue harvested from human donors) can be transplanted to restore meniscal function.
The same principles of restoration of load bearing applies to the hip joint, where the labrum (a C-shaped cartilage like structure that is important for load distribution and synovial fluid seal) is reconstructed using soft tissue from other parts of your body. This can also be performed with arthroscopic surgery.
Cartilage restoration techniques are essential in joint preserving surgery (Picture 3). These range from simple techniques like microfracture to more advanced techniques such as osteochondral transfers, matrix assisted cartilage repairs, cultured cartilage cells and osteochondral allografts. The detailed discussion of these various techniques is beyond the scope of this article, your surgeon will decide which technique is most suitable for you. Your age, size and depth of the cartilage damage and the availability and cost of these methods are important in the decision making process.
A stable joint is a prerequisite for joint preservation. Damaged ligaments can be reconstructed with tissue from your own body or allografts (tissue from a human donor). Arthroscopic ligament reconstruction is a well established technique regardless of age of the patient. Technical modifications are needed in middle aged arthritic patients.
Most of the patients require a combination of the above mentioned techniques in the same setting. This is a complex procedure requiring a high level of surgical expertise for a satisfactory outcome. The patient should also be highly motivated and willing to undergo a long and complex recovery with physiotherapy, home exercises and gym work.
