Prof. N. Reha Tandoğan, M.D. - Asım Kayaalp, M.D.
What is Osteochondritis dissecans?
Osteochondritis dissecans is a disease in which a small fragment of bone adjacent to the cartilage in the knee joint separates from the surrounding bone due to a local problem in blood supply. The cartilage covering the fragment is still viable since it receives its nutrients from the joint fluid, while the bone below the cartilage is dead. In the early stages of the disease, the fragment lies in a crater in the surrounding bone, with weak soft tissue attachments and an intact cartilage. However, this fragment separates from the bone and becomes a freely moving loose body in the joint unless treated or healing occurs spontaneously in children.Osteochondritis dissecans is usually seen in children before adolescence. Most of the adult patients presenting with osteochondritis are untreated or unrecognized cases that manifest symptoms when the fragment separates from the underlying bone.
Where does Osteochondritis dissecans occur?
Osteochondritis dissecans is most commonly seen in the knee and ankle joints. Less frequently, hip and elbow joints are affected. It is more common in boys and both knees may be affected in 15-30% of the children. However, the symptom severity and disease progression may not be the same if both knees are affected, one knee may progress to healing while the other knee may require surgery.What are the symptoms of Osteochondritis dissecans?
The main symptom of osteochondritis dissecans is pain. This pain increases with sports and activity and decreases with rest. If the fragment has separated and a loose body is present, mechanical symptoms such as catching and locking may occur, some patients may feel the fragment moving around the joint. Swelling also occurs after separation.How is Osteochondritis dissecans diagnosed?
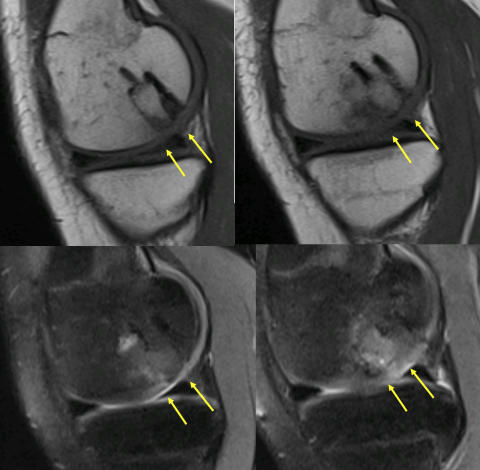
Osteochondritis dissecans can be diagnosed with a careful physical exam followed by plain X-rays in the majority of the patients (Figure 1). Advanced imaging methods such as computed tomography (CT) and magnetic resonance imaging (MRI) are needed for determining the stage of the disease, planning surgery and analyzing treatment outcomes (Figure 2) Arthroscopic examination is an essential part of the diagnosis, the joint is visualized using a 5 mm camera and the size, location, stability and suitability for repair of the fragment is determined. This is followed arthroscopic or open treatment of the disease.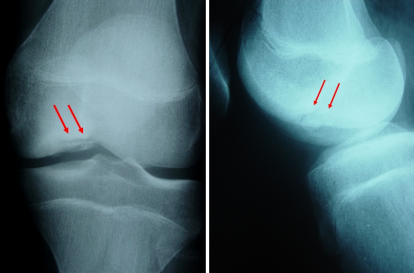
Can Osteochondritis dissecans heal without surgery?
Osteochondritis dissecans diagnosed before the end of adolescence has a potential for healing in more than half of the children without surgery (Figure 3). If the fragment is stable in its crater and the continuity of the cartilage cover is not compromised, the disease may progress to healing in about 2 years. Impact sports are avoided and MRI follow-up is made at 6-month intervals. Children with cartilage cracks and signs of early separation of the fragment in MRI’s need surgery. The prognosis of the disease is may not be the same for both knees. One side may heal spontaneously while the other may need surgery.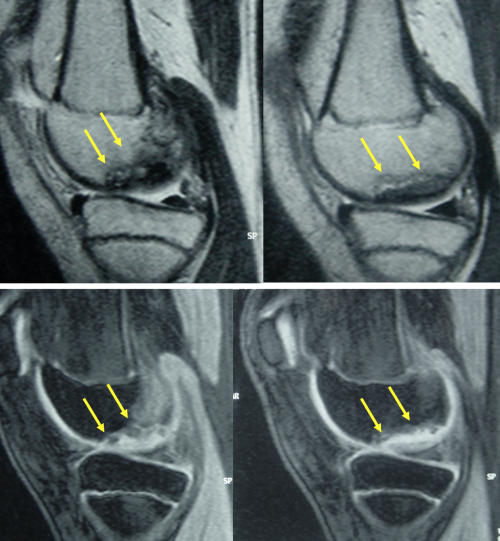
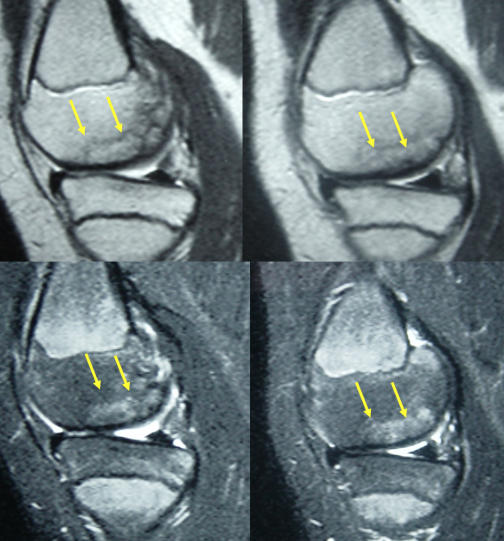
Figure 3 a,b: Healing of osteochondritis dissecans in a child before the end of adolescence. a: MRI’s at initial presentation; b: Healing without problem at 2 years.
Unlike children, adults with osteochondritis dissecans do not have a potential for spontaneous healing. These patients need surgery at the time of diagnosis.
What are the surgical treatment options for osteochondritis dissecans?
The choice of surgical treatment for osteochondritis dissecans depends on the size & location of the fragment, stage of the disease and age of the patient. All patients undergo an arthroscopic examination before deciding on the type of treatment.If the fragment is stable in its crater and the cartilage cover is intact, multiple drill holes are made through the fragment reaching deep into the surrounding healthy bone. These perforations provide tunnels for new cells and blood vessels to reach the diseased area and trigger a healing response.
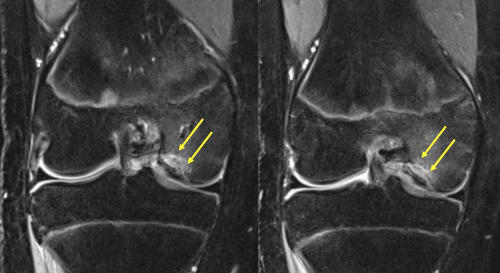
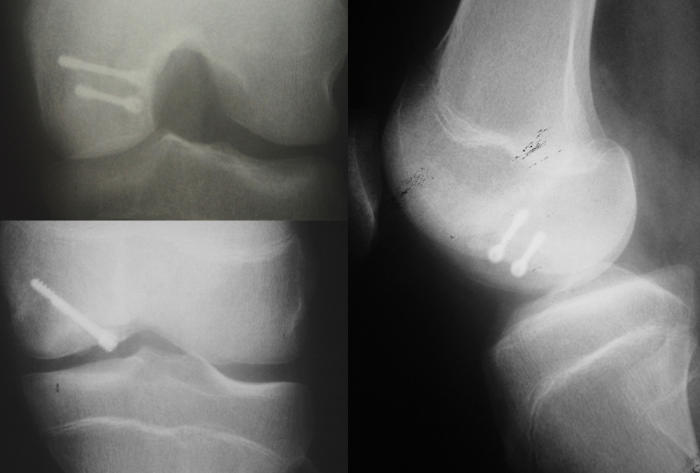
Fragments that are mobile in their craters but still attached to the underlying bone with soft tissue connections can be fixed with screws (Video 1). First the fragment is lifted out of its bed like a trapdoor, soft tissues impeding healing are removed and the bone surfaces are freshened. Bone chips harvested from the adjacent bones can be placed under the fragment to provide a perfect surface contour and a biological stimulus for healing. The fragment is placed back into its crater and fixed with two implants (Figure 4). Both metal and biodegradable screws/darts have been used for fixation. Metal implants provide better compression and stability but need to be removed after 3 months.
Video 1
Fragments that are too thin to provide adequate fixation or have been deformed while floating free in the joint cannot be fixed with implants. These fragments are removed and a procedure to reconstruct the bone and cartilage loss is selected. The most reliable method for this is called a “mosaicplasty” (Autologous osteochondral transplantation) in which bone plugs covered with cartilage are harvested from the non-weightbearing areas of the joint and are placed into the defect. (Figure 5).

How is the recovery after surgery?
Recovery after surgery for osteochondritis dissecans varies with the type of procedure. A 6 to 8 week period of partial weightbearing with crutches is usually needed. No cast of brace is necessary. Immediate knee motion and muscle strengthening exercises are started. Physiotherapy may rarely be needed. Healing is monitored with serial X-rays and an MRI’s (Figure 6). Return to sports is possible after full recovery, which not earlier than 6 months after surgery.