Prof. Dr. N. Reha Tandoğan - Op. Dr. Asım KayaalpThe widespread use of PRP (Platelet Rich Plasma) over the years have led to clear guidelines on indications and preparation methods. Until recently, PRP was an umbrella term used for all the platelet concentrates, and the efficacy of various products were thought to be similar, leading to many studies demonstrating no superiority in outcomes compared to placebo or alternative treatments. Commercial PRP kits differ in the volume of blood processed, concentration of platelets, presence or absence of leukocytes/monocytes, platelet yield and final volume of product. This has led to the novel concept of “platelet dose”, which is the total number of cells delivered to the injured or diseased tissue. The platelet dose for therapeutic effect may vary from site to site and may be different in the same location for different pathologies. Therefore, you should have a knowledgeable discussion with your doctor before deciding on the type of PRP treatment.
1. Ask if a closed PRP system will be used and inquire the rate of platelet concentration the PRP kit can achieve compared to baseline.
All PRP preparation systems follow the same protocol of sterile blood draw, processing of the blood to selectively isolate various cell types followed by sterile delivery of the final product via a syringe. All these steps should occur in a closed system, which means that the blood and its final products should have no contact with the outside environment until delivery. Low-cost open systems require the blood to be transferred from tube to tube several times and carry the risk of bacterial contamination and infection.
All commercially available PRP kits concentrate platelets to at least x2 of baseline. Current high quality PRP kits can concentrate platelets up to x6 - x8 of baseline. The platelet dose is correlated with outcomes, with higher doses leading to better outcomes that last longer. A recent comparison of various PRP kits is presented below, demonstrating the wide variability in the amount of cell concentration, volume and final platelet dose from a blood sample of the same patient (Adapted from Everts PA, Mazzola T, Mautner K, Randelli PS, Podesta L. Modifying Orthobiological PRP Therapies Are Imperative for the Advancement of Treatment Outcomes in Musculoskeletal Pathologies. Biomedicines. 2022 Nov 15;10(11):2933. doi: 10.3390/biomedicines10112933.)
| Angel | GPS III | Emcyte Pure PRP | PRF | Regenkit A | |
|---|---|---|---|---|---|
| Platelet increase from baseline | x4.8 | x4.2 | x6.6 | x1.9 | x0.7 |
| Platelet concentration (million/ml) | 856 | 754 | 1175 | 338 | 125 |
| Final product volume (ml) | 3 | 6 | 7 | 2 | 5 |
| Total platelet dose (million) | 2568 | 4524 | 8225 | 677 | 623 |
2. Ask about the maximum number of cells that the PRP system provides and if you would need more than one injection to achieve the desired effect
The number of platelets (ie. the platelet dose) has emerged as an important determinant of efficacy in the treatment of musculo-skeletal conditions. The combined analysis of multiple studies on the same subject by different authors (meta-analysis) have shown that different platelet doses are needed for the treatment of different conditions.Muscle-tendon, meniscus, plantar fascia conditions require a minimum platelet dose of 3.5 billion platelets. Studies with doses below this threshold have demonstrated no significant benefit of PRP, while studies over this threshold have shown marked efficacy. (Everts PA. Biomedicines. 2023 Jul 6;11(7):1922.)
In a similar fashion, 10 billion platelets have been demonstrated to have a significant and longer lasting effect compared to lower doses in the treatment of knee osteoarthritis (Berrigan W. Curr Rev Musculoskelet Med. 2024;17(12):570-588). If the PRP kit utilized cannot achieve this total platelet dose in a single procedure, multiple injections may be required.
3. Ask about the volume of blood draw and the final volume of the PRP product that will be injected.
Human blood contains 150.000-300.000 platelets/microliter. This is equivalent to 150-300 million platelets per milliliter. Even the most advanced systems have a platelet yield up to 90%, meaning some of the cells will be lost during the preparation process. This yield rate may be much lower in low-cost PRP kits. The volume of blood draw is important to achieve the final number of platelets in PRP. Higher initial blood volumes mean a greater number of baseline platelets that can be concentrated. If a therapeutic effect is desired with a single PRP injection for knee osteoarthritis, the minimum volume of blood draw should be 60 ml The final PRP volume is between 3-7 ml, this can be tailored to the volume that can safely be delivered to the injured/diseased area. PRP systems with 10-15ml initial blood draw volumes may require multiple injections to achieve the same effect.4. Ask about the presence and absence of leukocytes in the PRP product
Leukocytes are white blood cells that fight microorganisms, and their numbers increase in acute infections. They are also an important part of inflammation which is the first step of healing after injury. Leukocytes can be diluted/removed (Leukocyte Poor PRP, L-P PRP) or concentrated (Leukocyte Rich PRP, L-R PRP) depending on the type of PRP kit used. Both types of PRP have been used with mostly similar effects. However, Leukocyte Poor PRP is preferred in knee osteoarthritis where inflammation is not desired (Xiong Y. Front. Med. 2023; 10:1204144). In contrast, Leukocyte Rich PRP is useful when an inflammatory response is required, such as chronic non healing wounds, bone regeneration and chronic tendinopathies. (Le ADK. Curr Rev Musculoskelet Med. 2018 ;11(4):624-634). Several modern PRP kits allow the physician to adjust the concentration of leukocytes in the final PRP product, depending on the need for an inflammatory response in the injected area.
5. Ask how should you manage your blood thinning medication
Many patients requiring PRP treatment also use anti-aggregant or anti-coagulant medication such as Aspirin, Coraspin, Ecopirin, Plavix, Eliquis ect. These medications inhibit platelet function and may decrease the effectiveness of PRP treatment. Patients with a recent coronary stent or stroke cannot discontinue their blood thinning treatment due to life threatening consequences. Precautions should be undertaken to decrease the risk of bleeding in these patients & injections around the spinal cord should be avoided. Injections to the joints, muscles, tendons and the meniscus are relatively safe and can be performed, noting the risk of decreased effectiveness. Aspirin should be discontinued 10 days before and 10 days after the injection of PRP in patients using Aspirin prophylactically, without a defined risk of thrombosis.6. Ask if imaging such as ultrasound or fluoroscopy will be needed
The precise delivery of PRP to the injured/diseased is essential for efficacy. No additional imaging is required for the knee joint in experienced hands. If present, effusion (swelling of the joint due to excess joint fluid) should be evacuated before delivering the PRP to avoid dilution. Difficult to reach joints (such as the hip or thumb basal joint, facet joints of spine) or areas where external landmarks do not provide adequate information for targeted delivery (such as the rotator cuff, Achilles and patellar tendons, meniscus) may require additional imaging. Ultrasound is the most common modality but requires trained operators. Fluoroscopy (X-ray) may be needed for the hip & spinal facet joints.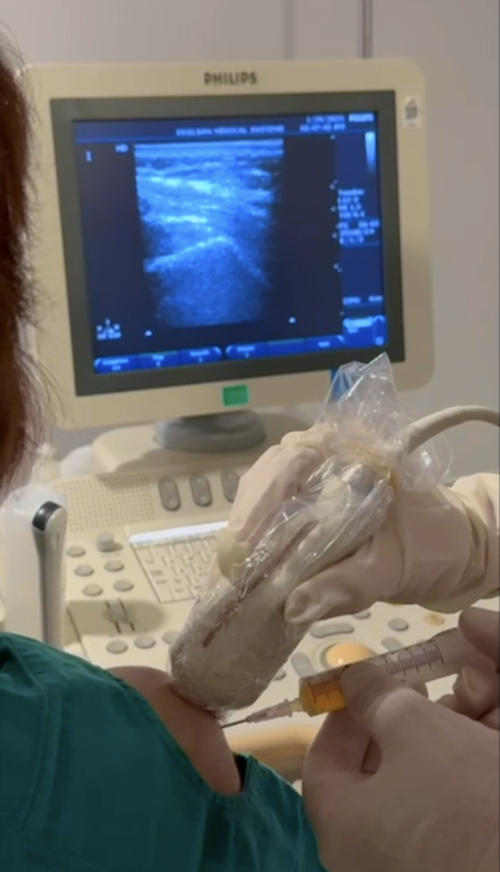
7. What should you know about the procedure itself?
The preparation and injection of PRP should be performed in strict sterile conditions. Depending on the system, 20-60 cc of venous blood is drawn and placed into the closed container of the PRP kit. Anticoagulant is added to prevent clotting. The kit is placed in a dedicated centrifuge and the cells are separated in layers in the PRP kit. This centrifuge process may take between 10 to 20 minutes; some systems perform a double spin in the centrifuge to further concentrate the cells. The final PRP is drawn into a syringe and is ready to be delivered. Studies have shown that the PRP product can be stored up to 4 hours at room temperature without a marked loss of biologic activity, however, injection as soon as possible is advised to ensure maximum biological activity and minimize the risk of contamination (Wilson BH. Am J Orthop (Belle Mead NJ). 2018;47(4)).Meanwhile, the area where PRP will be injected is prepared in a sterile fashion. Betadine, chlorhexidine or alcohol solution may be used for skin preparation, followed by placement of a sterile drape. The physician should wear sterile gloves throughout the procedure. Sterile draping of the ultrasound probe or fluoroscopy (X-ray) device is mandatory. Combination of PRP with local anesthetics or cortisone is not advised. Topical anesthetics or injection of local anesthetic medication only to the skin with a separate syringe may be performed for pain control. Combined injection with Hyaluronic acid into the joint has not been associated with detrimental effects.
Some pain and minimal swelling after injection of PRP may occur. Cold packs and application of ice may be helpful to decrease the pain. Paracetamol 3-4 times a day can be used as needed for pain. The use of non-steroidal anti-inflammatory medication should be avoided for 2-3 weeks if possible. Strenuous sports or aggressive weight lifting should be avoided for 3 weeks, this might be longer depending on the type of injury/disease.
